Thirst
By Professor Simon Thornton, Professor in Neurosciences at the Faculty of Sciences, University of Lorraine, Nancy, France.
Thirst
It is often said that thirst should be the guide for drinking, but what does it mean to be thirsty? Many people talk about this sensation, but few people can say that they actually feel it. Many authors have studied the physiological regulation of thirst, fluid intake and body fluids (1-6). Here we show you the physiology of the thirst mechanism making the body looking for liquid.
The distribution of water in the body
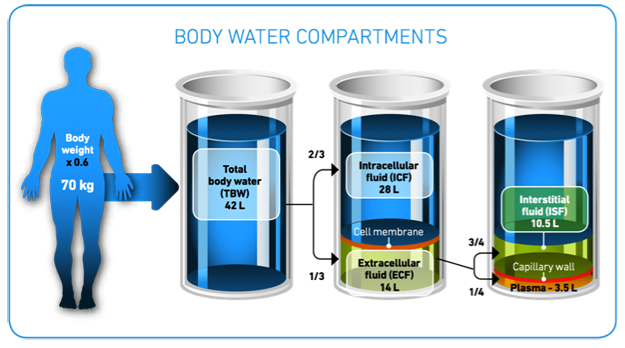
Our bodies are composed of a certain percentage of water, 70% when a baby going down to 55% or lower when aged. About two thirds of the water in the body is found within the cells (the intracellular space) and the rest is found in the extracellular space, which consists of the spaces between cells (the interstitial space) and the blood plasma (7) as shown below . These are not static volumes, and movement of water between the two major compartments (intracellular and extracellular ones, see figure) occurs depending on the concentration gradient between them. This means that when there is a difference in the concentration of the ions inside the cells from outside then water will move from the area of lower concentration until both areas are of the same concentration.
*Adapted from: Elsevier, Inc. Netterimages.com. http://www.netterimages.com/images/vpv/000/000/021/21248-0550×0475.jpg. See references in the text.
The ideal solute concentration inside our bodies is around 300 mosmol/L, which is equivalent to 9 g of sodium in a litre of water (e.g. similar to a solution of physiological saline that can be bought in any pharmacy). As sodium is the principal ion in the extracellular compartment this gives a reasonably accurate picture of what can happen inside the body. A loss of water in the body or an increased salt intake with eating produces an increase in the concentration of sodium in the extracellular compartment, so water leaves the cells down the concentration gradient.
The physiological response
Physiology of water homeostasis
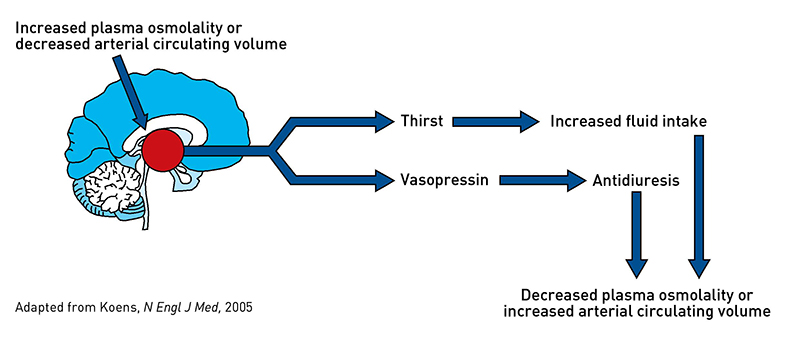
 i.e. the process of searching for and ingesting water as well as the release into the blood of antidiuretic hormone (ADH or vasopressin). As its names suggests ADH acts in the kidney to reduce the loss of water in the urine (antidiuresis) (8).
i.e. the process of searching for and ingesting water as well as the release into the blood of antidiuretic hormone (ADH or vasopressin). As its names suggests ADH acts in the kidney to reduce the loss of water in the urine (antidiuresis) (8).
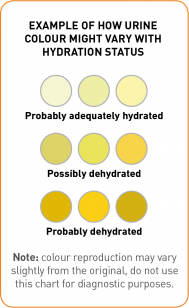
If water is drunk it then enters the blood supply via absorption in the gut and reduces the concentration gradient thus re-establishing the normal concentration in both compartments. This reduces the levels of ADH and allows the cells of the body to function normally and the kidney to produce urine again. If drinking does not occur rapidly, or not enough is consumed, then more and more ADH is released thus reducing more and more the production of urine. This usually can be seen in the smaller volumes of urine voided (i.e. going to the toilet less often) and this urine is often darker in colour than normal (9).
When too much water is lost
Loss of water specifically from the extracellular compartment can also occur (extreme examples with haemorrhage or vomiting ). This produces a decrease in blood volume and specialised cells in the cardiovascular system detect this decrease and signal the brain to release ADH and to increase the level of another hormone called angiotensin.
Angiotensin has several actions (10):
- it is vasoactive (i.e. it produces a decrease in the diameter of the blood vessels);
- it stimulates the release of ADH and the searching for and consumption of water;
- it stimulates the release of yet another hormone aldosterone.
The main action of aldosterone is to decrease the amount of sodium excreted in the urine (by reabsorption of sodium). All the actions of the volume receptors and of angiotensin are to try and ensure that water and sodium are retained so that the blood volume will not decrease to a level that is dangerous to health. If drinking of water is initiated, then blood volume will return to normal rapidly and the hormone levels will decrease, this allowing the body to function normally. If drinking does not occur or not enough is drunk, then more and more of the three hormones are produced, thus reducing more and more the volume of urine which will be increasingly darker in colour.
Why don’t humans always respond to these physiological signals of thirst?
This is a complex issue (6) and may depend on several factors such as (11):
- not knowing the benefits of fluid intake;
- not remembering to drink;
- disliking the taste of water;
- lack of thirst;
- lack of water availability;
- the need to void frequently and related workplace disruptions.
Cognitive assessment of toilet availability could play a role in decisions about when and where to drink despite the presence of physiological thirst signals.
Recent studies showing high urine osmolality, a sign of dehydration, in school children as they arrive at school suggests that limited access to the toilet could be one of the factors that influence children as to when they drink (12-14). It could be suggested that in humans there appears to be a form of cognitive control on responding to the thirst signals and perhaps this ability to override the signals leads in the long term to an inability to perceive correctly thirst, causing some individuals to stay hypohydrated for long periods throughout life.
When the thirst mechanism is impaired
Ability to feel thirst decreases with age, and certain medications can affect the hormonal response.
With age, the body loses its ability to have a thirst response to a fluid deficit, which increases the risk for dehydration. Therefore, in order to stay properly hydrated, elderly people should anticipate the body’s needs and not always wait until they are thirsty to have a drink (7).
Medications that are designed to block the production of angiotensin and/or to inhibit its specific receptor make up over 80% of treatments for hypertension and heart failure. Furthermore, these same medications can be used to treat other modern problems like obesity, diabetes, cancer and even Alzheimer’s disease (15). The release of angiotensin into the blood is the physiological response to dehydration of the extracellular compartment (16) so there could be a link between long-term mild dehydration and these modern health problems.
We would like to thanks Professor Simon Thornton, UHP, Nancy, France for providing the content used as a basis for the text in this section. His full scientific article entitled What is meant by thirst and why do we not feel the drive to drink when we are physiologically thirsty? can be found in our section Selected Articles.
1. Ramsay DJ. The importance of thirst in maintenance of fluid balance. Baillieres Clin Endocrinol Metab 1989; 3(2):371-91.
2. McKinley MJ, Johnson AK. The physiological regulation of thirst and fluid intake. News Physiol Sci 2004; 19:1-6.
3. Stricker EM, Hoffmann ML. Presystemic signals in the control of thirst, salt appetite, and vasopressin secretion. Physiol Behav 2007; 91(4):404-12.
4. Noakes TD. Is drinking to thirst optimum? Ann Nutr Metab. 2010;57 Suppl 2:9-17.
5. Thornton SN. Thirst and hydration: physiology and consequences of dysfunction. Physiol Behav 2010; 100(1):15-21.
6. Millard-Stafford M, Wendland DM, O’Dea NK, Norman TL. Thirst and hydration status in everyday life. Nutr Rev 2012;70 Suppl 2:S147-51.
7. EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA); Scientific Opinion on Dietary reference values for water. EFSA Journal 2010; 8(3):1459. Available at: www.efsa.europa.eu/en/efsajournal/pub/1459.htm
8. Knoers NVAM. Hyperactive vasopressin receptors and disturbed water homeostasis. N Engl J Med. 2005;352(18):1847-50.
9. Armstrong LE, Pumerantz AC, Fiala KA, Roti MW, Kavouras SA, Casa DJ, Maresh CM. Human hydration indices: acute and longitudinal reference values. Int J Sport Nutr Exerc Metab 2010; 20(2):145-53.
10. Fitzsimons JT. Angiotensin, thirst, and sodium appetite. Physiol Rev 1998; 78(3): 583-686
11. McCauley LR, Dyer AJ, Stern K, Hicks T, Nguyen MM. Factors influencing fluid intake behavior among kidney stone formers. J Urol. 2012;187(4):1282-6.
12. Bonnet F, Lepicard EM, Cathrin L, Letellier C, Constant F, Hawili N, Friedlander G. French children start their school day with a hydration deficit. Ann Nutr Metab 2012; 60(4):257-63.
13. Fadda R, Rapinett G, Grathwohl D, Parisi M, Fanari R, Calò CM, Schmitt J. Effects of drinking supplementary water at school on cognitive performance in children. Appetite 2012; 59(3):730-7.
14. Stookey JD, Brass B, Holliday A, Arieff A. What is the cell hydration status of healthy children in the USA? Preliminary data on urine osmolality and water intake. Public Health Nutr 2012; 15(11):2148-56.
15. Thornton SN. Angiotensin inhibition and longevity: a question of hydration. Pflugers Arch 2011; 461(3):317-24.
16. Damkjær M, Isaksson GL, Stubbe J, Jensen BL, Assersen K, Bie P. Renal renin secretion as regulator of body fluid homeostasis. Pflugers Arch. 2012 Oct 25. [Epub ahead of print]